Rest is a weapon; sleep deprivation decreases productivity in the office, and on the field. More than 1 out of every 3 Americans doesn’t get enough sleep [1].
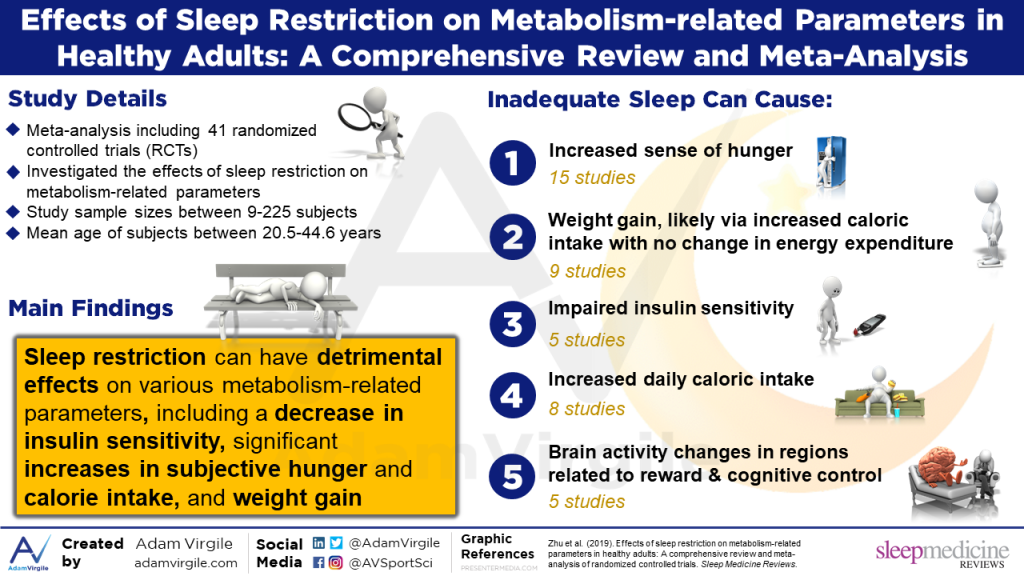
A study by Gradisar et al. (2013) found that a significant portion of adolescents (67%), young adults (67%), middle adults (65%), and older adults (58%) reported not getting enough sleep to function properly [2]. According to a meta-analysis of randomized controlled trials by Zhu et al. (2019), sleep restriction can also wreak havoc on metabolism, in healthy adults [55]. Lack of quality sleep can cause increased hunger, increased caloric intake, weight gain, impaired insulin sensitivity, and even activity changes in brain regions related to reward and cognitive control [55].
Athletes may be even more prone to sleep deprivation and limited daily function than the average person because they tend to have greater difficulty falling and staying asleep [3-6]. Because lack of sleep can result in athletic performance decrements, exercisers and athletes need to be particularly mindful of their sleep habits [7-11]. Even in youth athletes, lack of sleep has been associated with impaired self-reported well-being and increased injury risk [56, 57].
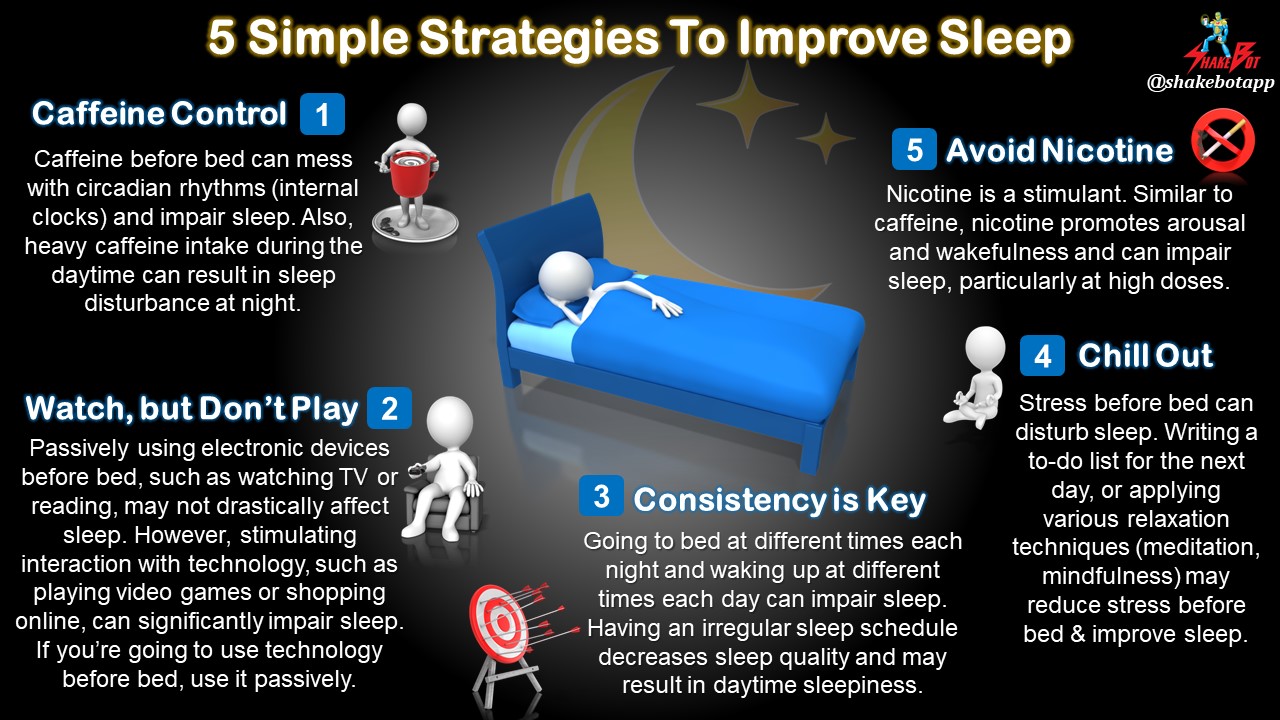
The importance of a solid night’s sleep, athlete or not, cannot be overstated. Use these 5 simple tips to get a better night’s sleep:
1. Caffeine Control
As little as 200mg of caffeine (equivalent to a double espresso) 3 hours before bed can disrupt sleep by interfering with circadian rhythms [12, 13]. It’s becoming clear that heavy caffeine intake, even just during the daytime, may result in sleep disturbance at night [14-18]. The interplay between heavy daytime caffeine consumption and disturbed sleep can turn into a vicious cycle: Disturbed sleep can lead to daytime sleepiness, which may cause heavy caffeine consumption the following day, coming full circle to disturbed sleep, once again, at night [14]. If you’re having trouble sleeping and consume substantial amounts of caffeine, it may be wise to take a hard look at the quantity and timing of your caffeine intake.
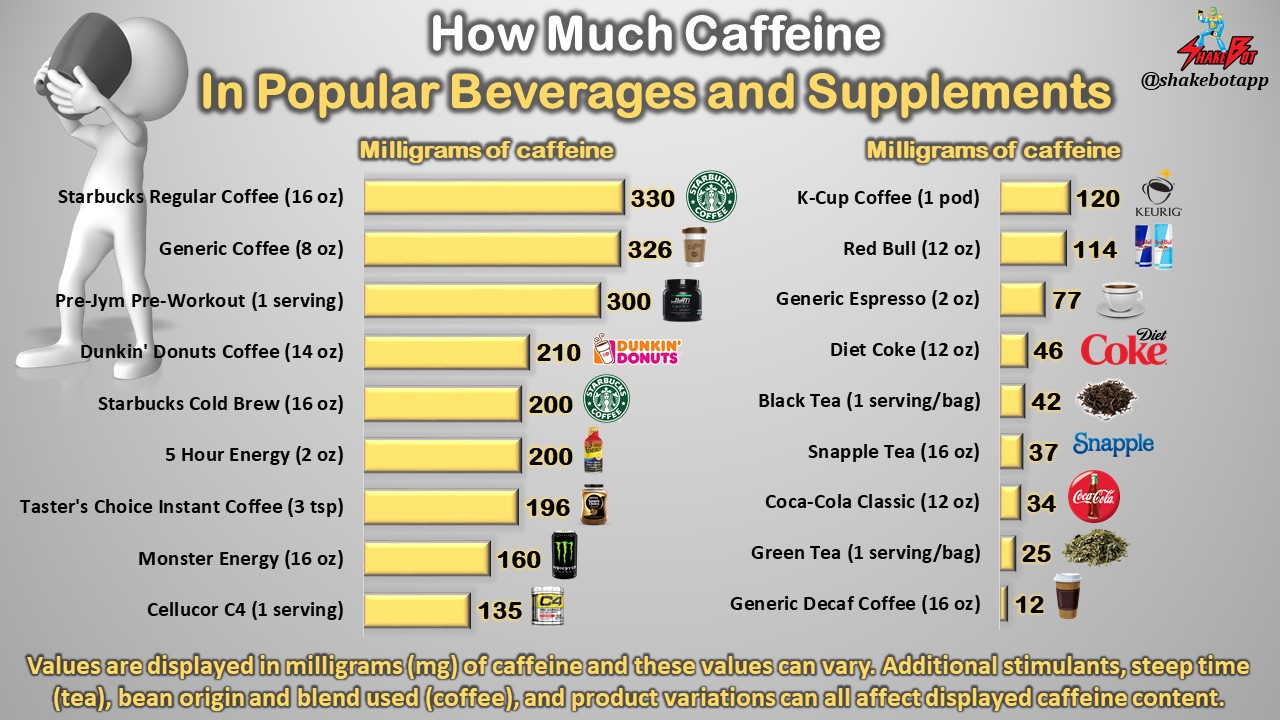
Note: If interested, you can also see graphics that breakdown the caffeine contents of different categories of products, such as popular coffee brands, teas, soft drinks, pre-workout supplements, and energy drinks.
2. Lay Off the Nicotine
Similar to caffeine, nicotine promotes arousal and wakefulness [19] which can impair sleep, particularly when taken (or used) at high doses [20, 21]. If you plan to stop smoking, going cold turkey may not be advisable if you smoke more than a pack a day. Habitual smokers who stop smoking abruptly can experience sleep disturbances, as well [22]. If you’re a habitual nicotine user who would like to improve sleep, try weaning off the substance rather than abruptly quitting altogether. At the very least, try to avoid nicotine close to bedtime.
3. “Chill Out”
Stress before bedtime can cause significant sleep disturbance [23-27]. Luckily, various stress management techniques can instantly reduce stress. To improve sleep, try writing a worry list or a to-do list for the next day, meditating, deep breathing, or practicing various other relaxation techniques before bed [28-31]. High levels of daytime stress can also impair sleep [32-34]. To reduce daytime stress, try practicing mindfulness, focusing on the present, laughing, interacting socially, or exercising; these techniques can drastically reduce daily stress and instantly improve sleep [35-38].
4. Toss the Tech: You May Watch, but Certainly Don’t Play
90% of Americans engage with technology in the hour before going to bed [2]. The type of technology used may matter more than the act of using technology itself. Researchers found that passively using electronic devices before bed, such as watching TV, reading, or listening to music, did not affect sleep [2]. However, stimulating interaction with technology, such as playing video games, browsing on the computer, or using a cell phone, significantly impaired sleep [2]. Whether it be from arousal [39-42], screen light [43, 44], or electronic transmissions [45], stimulating interactions with technology and sleep quality do not mesh well. New research indicates that the distance between you and your smartphone may impact sleep, as well [46]. Viewing distance in the lying position is shorter than that in the sitting position. It took students longer to fall asleep and their sleep efficiency was decreased when they spent time viewing their smartphones lying down (shorter viewing distance) before bed [46].
5. Consistency is Key
Going to bed at different times each night and waking up at different times each morning can impair sleep [47-50]. This is a common trait in insomniacs (i.e. people who habitually have trouble sleeping). In fact, having an irregular sleep schedule may cause daytime sleepiness [51] in addition to poor sleep quality [52, 53]. To optimize your sleep and performance, try your best to be on a consistent sleep-wake schedule [8, 54].
Summary
- Avoid heavy caffeine and/or nicotine intake during the day, and any stimulant intake at all in the few hours before bed.
- Reduce stress before bed to improve sleep: meditation, deep breathing, or writing a to-do and/or worry list before bed can help.
- Avoid stimulating technology before bed: playing video games, surfing the web, and using your cell phone are examples of what not to do if you’re trying to improve sleep. If you’re going to use technology, use it passively, instead. Watching TV, reading, or listening to music may not be as harmful to sleep quality.
- Stick to a consistent sleep schedule. Going to bed and waking up at around the same time each day can drastically enhance sleep.
Reference
- Liu, Y., 2016. Prevalence of healthy sleep duration among adults—United States, 2014. MMWR. Morbidity and mortality weekly report, 65.
- Gradisar, M., Wolfson, A.R., Harvey, A.G., Hale, L., Rosenberg, R. and Czeisler, C.A., 2013. The sleep and technology use of Americans: findings from the National Sleep Foundation’s 2011 Sleep in America poll. Journal of clinical sleep medicine: JCSM: official publication of the American Academy of Sleep Medicine, 9(12), p.1291.
- Halson, S., Appaneal, R., Peterson, K., Welvaert, M., Vlahovich, N., Hughes, D., Waddington, G. and Drew, M., 2017. High prevalence of poor sleep quality in athletes: Implications to staying healthy and performing. Journal of Science and Medicine in Sport, 20, p.e80.
- Gupta, L., Morgan, K. and Gilchrist, S., 2016. Does Elite Sport Degrade Sleep Quality? A Systematic Review. Sports Medicine, pp.1-17.
- Tuomilehto, H., Vuorinen, V.P., Penttilä, E., Kivimäki, M., Vuorenmaa, M., Venojärvi, M., Airaksinen, O. and Pihlajamäki, J., 2017. Sleep of professional athletes: underexploited potential to improve health and performance. Journal of sports sciences, 35(7), pp.704-710.
- Whitworth-Turner, C., Di Michele, R., Muir, I., Gregson, W. and Drust, B., 2018. A comparison of sleep patterns in youth soccer players and non-athletes. Science and Medicine in Football, 2(1), pp.3-8.
- Halson, S.L., 2014. Sleep in elite athletes and nutritional interventions to enhance sleep. Sports Medicine, 44(1), pp.13-23.
- Fullagar, H.H., Skorski, S., Duffield, R., Hammes, D., Coutts, A.J. and Meyer, T., 2015. Sleep and athletic performance: the effects of sleep loss on exercise performance, and physiological and cognitive responses to exercise. Sports medicine, 45(2), pp.161-186.
- Simpson, N.S., Gibbs, E.L. and Matheson, G.O., 2017. Optimizing sleep to maximize performance: implications and recommendations for elite athletes. Scandinavian journal of medicine & science in sports, 27(3), pp.266-274.
- Brandt, R., Bevilacqua, G.G. and Andrade, A., 2017. Perceived sleep quality, mood states, and their relationship with performance among Brazilian elite athletes during a competitive period. Journal of strength and conditioning research, 31(4), pp.1033-1039.
- Thun, E., Bjorvatn, B., Flo, E., Harris, A. and Pallesen, S., 2015. Sleep, circadian rhythms, and athletic performance. Sleep medicine reviews, 23, pp.1-9.
- Landolt, H.P., 2015. Caffeine, the circadian clock, and sleep. Science, 349(6254), pp.1289-1289.
- Burke, T.M., Markwald, R.R., McHill, A.W., Chinoy, E.D., Snider, J.A., Bessman, S.C., Jung, C.M., O’Neill, J.S. and Wright, K.P., 2015. Effects of caffeine on the human circadian clock in vivo and in vitro. Science translational medicine, 7(305), pp.305ra146-305ra146.
- Roehrs, T. and Roth, T., 2008. Caffeine: sleep and daytime sleepiness. Sleep medicine reviews, 12(2), pp.153-162.
- Clark, I. and Landolt, H.P., 2017. Coffee, caffeine, and sleep: A systematic review of epidemiological studies and randomized controlled trials. Sleep medicine reviews, 31, pp.70-78.
- Distelberg, B.J., Staack, A., Elsen, K.D.D. and Sabaté, J., The Effect of Coffee and Caffeine on Mood, Sleep, and Health-Related Quality of Life. Journal of Caffeine Research.
- Pollak, C.P. and Bright, D., 2003. Caffeine consumption and weekly sleep patterns in US seventh-, eighth-, and ninth-graders. Pediatrics, 111(1), pp.42-46.
- Pecotic, R., Valic, M., Kardum, G., Sevo, V., & Dogas, Z. (2008). Sleep habits of medical students, physicians and nurses regarding age, sex, shift work and caffeine consumption. Lijecnicki Vjesnik, 130(3–4), 87–91
- Boutrel, B. and Koob, G.F., 2004. What keeps us awake: the neuropharmacology of stimulants and wakefulness-promoting medications. SLEEP-NEW YORK THEN WESTCHESTER-, 27, pp.1181-1194.
- Jaehne, A., Loessl, B., Bárkai, Z., Riemann, D. and Hornyak, M., 2009. Effects of nicotine on sleep during consumption, withdrawal and replacement therapy. Sleep medicine reviews, 13(5), pp.363-377.
- Irish, L.A., Kline, C.E., Gunn, H.E., Buysse, D.J. and Hall, M.H., 2015. The role of sleep hygiene in promoting public health: A review of empirical evidence. Sleep medicine reviews, 22, pp.23-36.
- Hughes, J.R., 2007. Effects of abstinence from tobacco: valid symptoms and time course. Nicotine & Tobacco Research, 9(3), pp.315-327.
- Morin, C.M., Rodrigue, S. and Ivers, H., 2003. Role of stress, arousal, and coping skills in primary insomnia. Psychosomatic medicine, 65(2), pp.259-267.
- Åkerstedt, T., Kecklund, G. and Axelsson, J., 2007. Impaired sleep after bedtime stress and worries. Biological psychology, 76(3), pp.170-173.
- Hall, M., Vasko, R., Buysse, D., Ombao, H., Chen, Q., Cashmere, J.D., Kupfer, D. and Thayer, J.F., 2004. Acute stress affects heart rate variability during sleep. Psychosomatic medicine, 66(1), pp.56-62.
- Nielsen, T. and Levin, R., 2007. Nightmares: a new neurocognitive model. Sleep medicine reviews, 11(4), pp.295-310.
- Vandekerckhove, M. and Wang, Y.L., 2017. Emotion, emotion regulation and sleep: An intimate relationship. Aims Neuroscience, 5(1).
- Hauri, P.J., 1993. Consulting about insomnia: a method and some preliminary data. Sleep: Journal of Sleep Research & Sleep Medicine.
- Hauri, P.J., 1991. Case studies in insomnia. Springer Science & Business Media.
- Means, M.K., Lichstein, K.L., Epperson, M.T. and Johnson, C.T., 2000. Relaxation therapy for insomnia: nighttime and day time effects. Behaviour Research and Therapy, 38(7), pp.665-678.
- Lichstein KL, Riedel BW, Wilson NM, Lester KW, Aguillard RN. Relaxation and sleep compression for late-life insomnia: a placebo-controlled trial. J Consult Clin Psychol. 2001;69:227–39.
- Kim, E.J. and Dimsdale, J.E., 2007. The effect of psychosocial stress on sleep: a review of polysomnographic evidence. Behavioral sleep medicine, 5(4), pp.256-278.
- Hanson, M.D. and Chen, E., 2010. Daily stress, cortisol, and sleep: the moderating role of childhood psychosocial environments. Health Psychology, 29(4), p.394.
- Watson, A.M., 2017. Sleep and athletic performance. Current sports medicine reports, 16(6), pp.413-418.
- Grossman, P., Niemann, L., Schmidt, S. and Walach, H., 2004. Mindfulness-based stress reduction and health benefits: A meta-analysis. Journal of psychosomatic research, 57(1), pp.35-43.
- Brand, S., Holsboer-Trachsler, E., Naranjo, J.R. and Schmidt, S., 2012. Influence of mindfulness practice on cortisol and sleep in long-term and short-term meditators. Neuropsychobiology, (3), pp.109-118.
- Caldwell, K., Emery, L., Harrison, M. and Greeson, J., 2011. Changes in mindfulness, well-being, and sleep quality in college students through taijiquan courses: a cohort control study. The Journal of alternative and complementary medicine, 17(10), pp.931-938.
- Ong, J.C., Shapiro, S.L. and Manber, R., 2008. Combining mindfulness meditation with cognitive-behavior therapy for insomnia: a treatment-development study. Behavior therapy, 39(2), pp.171-182.
- Mathiak, K. and Weber, R., 2006. Toward brain correlates of natural behavior: fMRI during violent video games. Human brain mapping, 27(12), pp.948-956.
- Weaver, E., Gradisar, M., Dohnt, H., Lovato, N. and Douglas, P., 2010. The effect of presleep video-game playing on adolescent sleep. J Clin Sleep Med, 6(2), pp.184-189.
- Higuchi, S., Motohashi, Y., Liu, Y. and Maeda, A., 2005. Effects of playing a computer game using a bright display on presleep physiological variables, sleep latency, slow wave sleep and REM sleep. Journal of sleep research, 14(3), pp.267-273.
- Ivarsson, M., Anderson, M., Åkerstedt, T. and Lindblad, F., 2009. Playing a violent television game affects heart rate variability. Acta paediatrica, 98(1), pp.166-172.
- Cajochen, C., Frey, S., Anders, D., Späti, J., Bues, M., Pross, A., Mager, R., Wirz-Justice, A. and Stefani, O., 2011. Evening exposure to a light-emitting diodes (LED)-backlit computer screen affects circadian physiology and cognitive performance. Journal of Applied Physiology, 110(5), pp.1432-1438.
- Chang, A.M., Aeschbach, D., Duffy, J.F. and Czeisler, C.A., 2015. Evening use of light-emitting eReaders negatively affects sleep, circadian timing, and next-morning alertness. Proceedings of the National Academy of Sciences, 112(4), pp.1232-1237.
- Wood, A.W., Loughran, S.P. and Stough, C., 2006. Does evening exposure to mobile phone radiation affect subsequent melatonin production?. International journal of radiation biology, 82(2), pp.69-76.
- Yoshimura, M., Kitazawa, M., Maeda, Y., Mimura, M., Tsubota, K. and Kishimoto, T., 2017. Smartphone viewing distance and sleep: an experimental study utilizing motion capture technology. Nature and science of sleep, 9, p.59.
- Stepanski, E.J. and Wyatt, J.K., 2003. Use of sleep hygiene in the treatment of insomnia. Sleep medicine reviews, 7(3), pp.215-225.
- Dijk, D.J. and Lockley, S.W., 2002. Invited Review: Integration of human sleep-wake regulation and circadian rhythmicity. Journal of applied physiology, 92(2), pp.852-862.
- Jefferson, C.D., Drake, C.L., Scofield, H.M., Myers, E., McClure, T., Roehrs, T. and Roth, T., 2005. Sleep hygiene practices in a population-based sample of insomniacs. Sleep, 28(5), pp.611-615.
- Buysse, D.J., Cheng, Y., Germain, A., Moul, D.E., Franzen, P.L., Fletcher, M. and Monk, T.H., 2010. Night-to-night sleep variability in older adults with and without chronic insomnia. Sleep medicine, 11(1), pp.56-64.
- Billiard, M., Alperovitch, A., Perot, C. and Jammes, A., 1987. Excessive daytime somnolence in young men: prevalence and contributing factors. Sleep: Journal of Sleep Research & Sleep Medicine.
- Carney, C.E., Edinger, J.D., Meyer, B., Lindman, L. and Istre, T., 2006. Daily activities and sleep quality in college students. Chronobiology international, 23(3), pp.623-637.
- Monk, T.H., Buysse, D.J., Billy, B.D., Fletcher, M.E., Kennedy, K.S., Schlarb, J.E. and Beach, S.R., 2011. Circadian type and bed-timing regularity in 654 retired seniors: correlations with subjective sleep measures. Sleep, 34(2), p.235.
- Phillips, A.J., Clerx, W.M., O’Brien, C.S., Sano, A., Barger, L.K., Picard, R.W., Lockley, S.W., Klerman, E.B. and Czeisler, C.A., 2017. Irregular sleep/wake patterns are associated with poorer academic performance and delayed circadian and sleep/wake timing. Scientific Reports, 7.
- Zhu, B., Shi, C., Park, C.G., Zhao, X. and Reutrakul, S., 2019. Effects of sleep restriction on metabolism-related parameters in healthy adults: A comprehensive review and meta-analysis of randomized controlled trials. Sleep Medicine Reviews.
- Watson, A. and Brickson, S., 2018. Impaired Sleep Mediates the Negative Effects of Training Load on Subjective Well-Being in Female Youth Athletes. Sports Health, 10(3), pp.244-249.
- Von Rosen, P., Frohm, A., Kottorp, A., Friden, C. and Heijne, A., 2017. Too little sleep and an unhealthy diet could increase the risk of sustaining a new injury in adolescent elite athletes. Scandinavian Journal of Medicine & Science in Sports, 27(11), pp.1364-1371.