Eating disorders are considerably more prevalent in the athletic community than in the general population [1]. This makes the identification of athletes with eating disorders, and those at risk for developing eating disorders, particularly important.
Blue boxes give more detail about key terms or subjects
Grey boxes are key points
Prevalence of Eating Disorders in Athletes
In 2004, Sundgot-Borgen and colleagues assessed the frequency of eating disorders in a sample of 1259 Norwegian male and female athletes and non-athlete controls. They found that a significantly higher proportion of athletes had an eating disorder, compared non-athlete controls [1]. The most common eating disorders included anorexia nervosa, bulimia nervosa, binge eating disorder, and anorexia athletica [1]. In females, prevalence of eating disorders has been reported to be 2-3x higher in athletes, compared with non-athlete controls [1, 2]. Females appear to be at a higher risk than males within the athletic population, as well. In a study of 638 NCAA Division I cross country and track distance running student-athletes, Krebs et al. (2018) recently found that the prevalence of eating disorders was substantially higher in the female athletes, compared with their male counterparts [3]. Eating disorder rates are profoundly higher in aesthetic and weight-dependent sports in both females, and males [1, 4, 5]. In some studies, up to 70% of athletes in weight class sports were dieting or exhibiting abnormal eating behavior to lose weight prior to competition [6]. In fact, according to a recent study by Voelker et al. (2018), having a sense of external pressure about weight was associated with eating disorder prevalence in male figure skaters [40]. I’d like to divert the focus towards the most well-known disordered eating trifecta in sport; the female athlete triad.

The Female Athlete Triad
The Female Athlete Triad (“the Triad”): An interrelationship between 1) menstural dysfunction, 2) low bone mineral density, and 3) low energy availability. In 2014, it was expanded upon, and redefined by a panel of experts and the American College of Sports Medicine as RED-S, or relative energy deficiency in sport.
In 2007, the American College of Sports Medicine released a position stand where the authors classify the components of the Female Athlete Triad, or “the Triad”, for short [17]. “The Triad”, has been characterized by 1) low energy availability, with or without disordered eating, 2) menstrual dysfunction, and 3) low bone mineral density [17]. The prevalence of the Triad in “lean sports” (those that emphasize weight categories or aesthetics, such as ballet, gymnastics, or endurance running) is 2-3x higher than in non-lean sports [17]. A recent review by Gibbs et al. (2013) examined the prevalence of the Triad in athletes across all levels of activity, and reported a relatively small percentage exhibiting all 3 triad conditions (0%-15.9%), but the prevalence of any 2 or any 1 of the Triad conditions ranged from 2.7% to 27.0% and 16.0% to 60.0%, respectively [18]. Yes, up to 60% of female athletes can be experiencing a facet of the Triad. One may think that nutritional knowledge (or lack thereof) is a potential reason for this phenomena. However, as demonstrated by Raymond-Barker et al. (2007), lack of nutritional knowledge is likely not the culprit [19]. The authors found that, despite female athletes being at higher risk for one or more components of the Triad, there were no differences in nutritional knowledge between the female athletes and their non-athlete counterparts [19]. Although not a statistically significant difference, the average nutritional knowledge score was actually higher in the athletic cohort [19]. There’s further evidence suggesting that acquiring adequate nutritional knowledge probably won’t change dietary behavior in female athletes [20, 21]. With that being said, lack of knowledge regarding the negative health consequences of the Triad could, potentially, be a contributor to the prevalence of the disorder [22].
Common signs and symptoms observed in the Triad include: rapid weight loss, eating restriction or routine fasting, and use of diet pills; cessation of menstruation in a eumenorrheic female; stress fractures; and overuse injuries that heal more slowly than anticipated. Athletes will often attempt to hide their illness or disorder, and thus, conversing with the athlete on a consistent basis is the best tool a coach has for assessing if/when something is off-kilter.
Coaches, parents, health care professionals, and fellow teammates should be aware of any of the signs and symptoms above, and discuss any concerns with the athlete privately [25]. Thein-Nissenbaum Hammer (2017) recently put together a fantastic in-depth resource that outlines signs, symptoms, diagnoses, and treatment strategies for young females experiencing the Triad [25]. For a comprehensive review, I suggest viewing their work.
Mountjoy et al. (2014) reveal scientific advances since 2007, which led the American College of Sports Medicine to redefine the Female Athlete Triad (menstrual dysfunction, low bone density, and low energy) to RED-S, or relative energy deficiency in sport.
Relative Energy Deficiency in Sport (RED-S)
Also in 2014, a panel of experts assembled by the International Olympic Committee proposed an expanded conceptualization of the Triad under the term “relative energy deficiency in sport”, [35]. The syndrome of “relative energy deficiency in sport”, or RED-S, represents an expansion beyond the mere three entities of “the Triad” (energy availability, menstrual function and bone health) in that it is a syndrome that can affect many aspects of physiological function, health and athletic performance.
In 2018, the panel of experts from the International Olympic Committee reconvened to provide an updated summary of the interim scientific progress in the field of RED-S [41]. I strongly advise giving this paper a read.
RED-S refers to impaired physiological function including, but not limited to, metabolic rate, menstrual function, bone health, immunity, protein synthesis, cardiovascular health caused by relative energy deficiency [35]. If the term “relative energy deficit in sport” is new to you, you’re not alone. Kroshus et al. (2018) conducted a recent survey in 285 NCAA head athletic trainers, and only 1/3 of the trainers had heard of the term “relative energy deficiency in sport,” despite the trainers having been certified in athletic training for 18 years, on average [39]. Although this disorder has been historically titled “the female athlete triad,” males are very prone to adopting disordered eating patterns and/or RED-S, as well as females.
Disordered Eating in Males
Although male athletes have a lower prevalence of disordered eating than female athletes, they still have a far higher prevalence than male non-athletes [7]. The pattern of medical conditions seen in the male athlete appears analogous to that seen in female athletes diagnosed with the Triad [23]. These conditions include low energy availability with or without disordered eating, reduced sex steroids including testosterone, and impaired bone health [23]. Regardless of the terminology used to describe it, it’s clear that energy balance is a critical element of athlete health and performance. Male adolescent athletes competing in ball or team sports such as football, soccer, and ice hockey tend to have sufficient energy intakes [7-10]. Periods of inadequate energy intakes and/or nutrient deficiencies are observed in athletes participating in sports that emphasize leanness or weight restriction (wrestling, judo, horse-racing) [12-14]. Burke et al. (2018) have a fascinating commentary where they delve into the details regarding specific cohorts of elite male athletes who demonstrate an elevated risk of low energy availability [43].
Given the increased energy demands that athletes have, compared with their non-athletic counterparts, athletes are more prone to developing an imbalance between energy intake and expenditure (both males, and females). Despite exercising 5x more hours/week, energy intake in adolescent male cyclists was comparable to that of their control counterparts, which failed to meet their dietary requirements [37]. Additionally, intake of important vitamins and minerals like calcium, vitamin D, iron, and B vitamins, were below recommendations for both cyclists, and controls [37]. Another study among 61 male cyclists demonstrated comparable results; the cyclists had elevated disordered eating behaviors compared with age-matched controls and exhibited poor intake of each food group compared with nutritional recommendations [38]. There’s further evidence that suggests that eating disorders and body dissatisfaction in male endurance athletes, including runners [26, 27] and triathletes [28], is more common than in non-athlete controls.
Educating coaches, and particularly male coaches, on eating disorders and optimal nutrition for sport may be a crucial aspect for reducing athlete disordered eating risk. Kroshus et al. (2014) conducted a survey in 227 high school coaches of female athletes, and found a significant difference in coaching practices and nutritional knowledge was found between male and female coaches [36]. Male coaches were more likely than female coaches to talk to athletes about eliminating certain foods from their diets and about achieving an ideal body for performance in their sport. Male coaches were also less likely to believe that skipping one or two meals per day was a threat to health or performance [36]. Although this study focused on coaches of female athletes only, it would be a mistake to assume that the research couldn’t also apply to coaches of male athletes. Research by Martinsen et al. (2015) suggests that a little bit of education may be helpful for coaches. Two, 3-hour education seminars improved awareness and knowledge of disordered eating in elite sport coaches [44]. Caudill (2018) implemented a single, 20-minute education session in 23 athletic staff members. She found that this brief education session resulted in a positive change in staff’s beliefs, attitudes, and behaviors related to disordered eating, as well as an increase in staff’s perception of seriousness of several disordered eating behaviors [45].
Summary and Practical Applications
Eating disorders are devastating psychiatric conditions. Eating disorders have an unacceptably high mortality rate and invoke considerable morbidity among those affected [29]. Given the pressure to achieve a body composition that optimizes athletic performance, athletes are at a greater risk than the general population for development of eating disorders [1]. Although females are typically affected more commonly than males [1], both sexes are at risk, particularly in sports where leanness offers a competitive athletic advantage [1,2, 15, 30-33]. To prevent and treat disordered eating, it’s essential that unwavering support for athlete health is consistent across the multidisciplinary team (coaches, administrators, trainers, teammates, parents, etc.). The National Collegiate Athletic Association (NCAA) has developed educational materials for coaches, athletic administrators and athletes in an effort to prevent eating disorders; 10 strategies that aim to reduce the likelihood of disordered eating are listed below [7]:
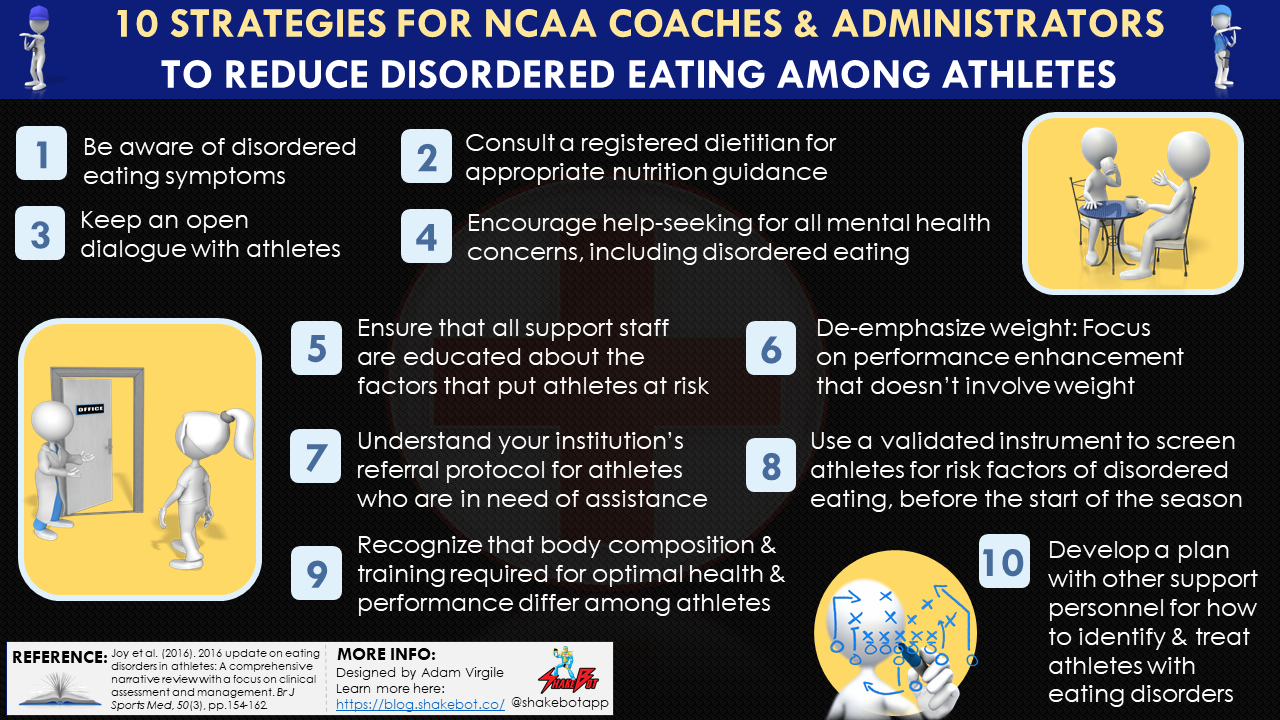
- Be aware of the symptoms of disordered eating.
- Consult a registered dietitian who specializes in sport, particularly a Board Certi?ed Specialist in Sports Dietetics (CSSD) to prescribe appropriate nutrition for optimal sport performance.
- De-emphasize weight: Be aware of how you are communicating to athletes about weight and performance. Focus on ways for athletes to enhance their performance that do not involve weight.
- Keep an open dialogue with athletes about the importance of nutrition and staying injury-free for optimal athletic performance.
- Recognize that body composition and training required for optimal health and performance is not identical for all athletes.
- Screen student-athletes before the start of the season for risk factors of disordered eating using a validated screening instrument.
- Ensure that all stakeholders (coaches, strength and conditioning coaches, athletic trainers, student-athletes, student-athlete affairs administrators and athletics department staff) are educated about the factors that put athletes at risk for disordered eating.
- Understand your institution’s referral protocol for student-athletes who are in need of assistance with nutrition or disordered eating issues.
- Encourage help-seeking for all mental health concerns, including disordered eating.
- Develop a plan with other stakeholders (such as university counseling services or a sports registered dietitian) for ways to identify and treat student-athletes with eating disorders.
For treatment protocols for the Triad, please refer to an in-depth 2014 consensus statement on the topic [24]. In any case, it’s imperative that an individualized program is used to provide appropriate care for an athlete experiencing an eating disorder, of any kind [42].
Reference:
- Sundgot-Borgen, J. and Torstveit, M.K., 2004. Prevalence of eating disorders in elite athletes is higher than in the general population. Clinical Journal of Sport Medicine, 14(1), pp.25-32.
- Sundgot-Borgen, J., 1993. Prevalence of eating disorders in elite female athletes. International Journal of Sport Nutrition, 3(1), pp.29-40.
- Thiemann, P., Legenbauer, T., Vocks, S., Platen, P., Auyeung, B. and Herpertz, S., 2015. Eating disorders and their putative risk factors among female German professional athletes. European Eating Disorders Review, 23(4), pp.269-276.
- Reinking, M.F. and Alexander, L.E., 2005. Prevalence of disordered-eating behaviors in undergraduate female collegiate athletes and nonathletes. Journal of Athletic Training, 40(1), p.47.
- Krebs, P.A., Dennison, C.R., Kellar, L. and Lucas, J., 2019. Gender Differences in Eating Disorder Risk among NCAA Division I Cross Country and Track Student-Athletes. Journal of Sports Medicine, 2019.
- Sundgot-Borgen J, Torstveit MK. Aspects of disordered eating continuum in elite high intensity sports. Scand J Med Sci Sports 2010;20(Suppl 2):112–21.
- Joy, E., Kussman, A. and Nattiv, A., 2016. 2016 update on eating disorders in athletes: A comprehensive narrative review with a focus on clinical assessment and management. Br J Sports Med, 50(3), pp.154-162.
- Rankinen T, Fogelholm M, Kujala U, Rauramaa R, Uusitupa M. Dietary intake and nutritional status of athletic and nonathletic children in early puberty. Int J Sport Nutr. 1995;5(2):136–50.
- Hickson JF Jr, Duke MA, Risser WL, Johnson CW, Palmer R, Stockton JE. Nutritional intake from food sources of high school football athletes. J Am Diet Assoc. 1987;87(12):1656–9.
- Rico-Sanz J, Frontera WR, Mole PA, Rivera MA, Rivera-Brown A, Meredith CN. Dietary and performance assessment of elite soccer players during a period of intense training. Int J Sport Nutr. 1998;8(3):230–40.
- Petrie HJ, Stover EA, Horswill CA. Nutritional concerns for the child and adolescent competitor. Nutrition. 2004;20(7–8): 620–31
- Dolan E, O’Connor H, McGoldrick A, O’Loughlin G, Lyons D, Warrington G. Nutritional, lifestyle, and weight control practices of professional jockeys. J Sports Sci. 2011;29(8):791–9.
- Horswill CA, Park SH, Roemmich JN. Changes in the protein nutritional status of adolescent wrestlers. Med Sci Sports Exerc. 1990;22(5):599–604.
- Fogelholm GM, Koskinen R, Laakso J, Rankinen T, Ruokonen I. Gradual and rapid weight loss: effects on nutrition and performance in male athletes. Med Sci Sports Exerc. 1993;25(3): 371–7.
- Chatterton JM, Petrie TA. Prevalence of disordered eating and pathogenic weight control behaviors among male collegiate athletes. Eat Disord. 2013;21(4):328–41.
- van Erp-Baart AM, Saris WH, Binkhorst RA, Vos JA, Elvers JW. Nationwide survey on nutritional habits in elite athletes. Part I. Energy, carbohydrate, protein, and fat intake. Int J Sports Med. 1989;10(Suppl 1):S3–10.
- Nattiv, A., Loucks, A.B., Manore, M.M…., and American College of Sports Medicine.American College of Sports Medicine position stand: the female athlete triad. Med Sci Sports Exerc. 2007; 39: 1867–1882
- Gibbs, J.C., Williams, N.I. and De Souza, M.J., 2013. Prevalence of individual and combined components of the female athlete triad. Medicine & Science in Sports & Exercise, 45(5), pp.985-996.
- Raymond-Barker, P., Petroczi, A. and Quested, E., 2007. Assessment of nutritional knowledge in female athletes susceptible to the Female Athlete Triad syndrome. Journal of Occupational Medicine and Toxicology, 2(1), p.10.
- Day, J., Wengreen, H., Heath, E. and Brown, K., 2015. Prevalence of low energy availability in collegiate female runners and implementation of nutrition education intervention. Sports Nutr Ther, 1(101), p.2.
- Miracle, A.L., 2013. Evaluation of the Relationship between Nutrition Knowledge and Disordered Eating Risk in Female Collegiate Athletes
- Miller, S.M., Kukuljan, S., Turner, A.I., van der Pligt, P. and Ducher, G., 2012. Energy deficiency, menstrual disturbances, and low bone mass: what do exercising Australian women know about the female athlete triad?. International Journal of Sport Nutrition and Exercise Metabolism, 22(2), pp.131-138.
- Tenforde, A.S., Barrack, M.T., Nattiv, A. and Fredericson, M., 2016. Parallels with the female athlete triad in male athletes. Sports Medicine, 46(2), pp.171-182.
- De Souza, M.J., Nattiv, A., Joy, E., Misra, M., Williams, N.I., Mallinson, R.J., Gibbs, J.C., Olmsted, M., Goolsby, M. and Matheson, G., 2014. 2014 Female Athlete Triad Coalition Consensus Statement on treatment and return to play of the female athlete triad: 1st International Conference held in San Francisco, California, May 2012 and 2nd International Conference held in Indianapolis, Indiana, May 2013. Br J Sports Med, 48(4), pp.289-289.
- Thein-Nissenbaum, J. and Hammer, E., 2017. Treatment strategies for the female athlete triad in the adolescent athlete: current perspectives. Open Access Journal of Sports Medicine, 8, p.85.
- Tenforde, A.S., Sayres, L.C., McCurdy, M.L., Collado, H., Sainani, K.L. and Fredericson, M., 2011. Overuse injuries in high school runners: lifetime prevalence and prevention strategies. PM&R, 3(2), pp.125-131.
- Wheeler, G.D., Wall, S.R., Belcastro, A.N., Conger, P. and Cumming, D.C., 1986. Are anorexic tendencies prevalent in the habitual runner?. British Journal of Sports Medicine, 20(2), pp.77-81.
- DeBate, R.D., Wethington, H. and Sargent, R., 2002. Sub-clinical eating disorder characteristics among male and female triathletes. Eating and Weight Disorders-Studies on Anorexia, Bulimia and Obesity, 7(3), pp.210-220.
- Arcelus, J., Mitchell, A.J., Wales, J. and Nielsen, S., 2011. Mortality rates in patients with anorexia nervosa and other eating disorders: a meta-analysis of 36 studies. Archives of General Psychiatry, 68(7), pp.724-731.
- Melin, A., Torstveit, M.K., Burke, L., Marks, S. and Sundgot-Borgen, J., 2014. Disordered eating and eating disorders in aquatic sports. International Journal of Sport Nutrition and Exercise metabolism, 24(4), pp.450-459.
- Rosendahl, J., Bormann, B., Aschenbrenner, K., Aschenbrenner, F. and Strauss, B., 2009. Dieting and disordered eating in German high school athletes and non?athletes. Scandinavian Journal of Medicine & Science in Sports, 19(5), pp.731-739.
- Thiel, A., Gottfried, H. and Hesse, F.W., 1993. Subclinical eating disorders in male athletes. Acta Psychiatrica Scandinavica, 88(4), pp.259-265.
- Kong, P. and Harris, L.M., 2015. The sporting body: body image and eating disorder symptomatology among female athletes from leanness focused and nonleanness focused sports. The Journal of Psychology, 149(2), pp.141-160.
- Kroshus E. “10 Eating Disorders Awareness Tips for Coaches and Athletics Professionals.” 23 Febuary 2015. http://www.ncaa.org/health-and-safety/ sport-science-institute/10-eating-disorders-awareness-tips-coaches-and-athleticsprofessionals (accessed 25 Oct 2015).
- Mountjoy, M., Sundgot-Borgen, J., Burke, L., Carter, S., Constantini, N., Lebrun, C., Meyer, N., Sherman, R., Steffen, K., Budgett, R. and Ljungqvist, A., 2014. The IOC consensus statement: beyond the female athlete triad—Relative Energy Deficiency in Sport (RED-S). Br J Sports Med, 48(7), pp.491-497.
- Kroshus, E., Sherman, R.T., Thompson, R.A., Sossin, K. and Austin, S.B., 2014. Gender differences in high school coaches’ knowledge, attitudes, and communication about the female athlete triad. Eating Disorders, 22(3), pp.193-208.
- Julian-Almarcegui, C., Gómez-Cabello, A., González-Agüero, A., Olmedillas, H., Gomez-Bruton, A., Matute-Llorente, A., Casajus, J.A. and Vicente-Rodríguez, G., 2013. The nutritional status in adolescent Spanish cyclists. Nutricion Hospitalaria, 28(4).
- Riebl, S.K., Subudhi, A.W., Broker, J.P., Schenck, K. and Berning, J.R., 2007. The prevalence of subclinical eating disorders among male cyclists. Journal of the American Dietetic Association, 107(7), pp.1214-1217.
- Kroshus, E., DeFreese, J.D. and Kerr, Z.Y., 2018. Collegiate Athletic Trainers’ Knowledge of the Female Athlete Triad and Relative Energy Deficiency in Sport. Journal of Athletic Training, 53(1), pp.51-59.
- Voelker, D.K., Petrie, T.A., Reel, J.J. and Gould, D., 2018. Frequency and psychosocial correlates of eating disorder symptomatology in male figure skaters. Journal of Applied Sport Psychology, 30(1), pp.119-126.
- Mountjoy, M., Sundgot-Borgen, J.K., Burke, L.M., Ackerman, K.E., Blauwet, C., Constantini, N., Lebrun, C., Lundy, B., Melin, A.K., Meyer, N.L. and Sherman, R.T., 2018. IOC consensus statement on relative energy deficiency in sport (RED-S): 2018 update. Br J Sports Med, 52(11), pp.687-697.
- Mountjoy, M.L., Burke, L.M., Stellingwerff, T. and Sundgot-Borgen, J., 2018. Relative energy deficiency in sport: the tip of an iceberg.
- Burke, L.M., Close, G.L., Lundy, B., Mooses, M., Morton, J.P. and Tenforde, A.S., 2018. Relative energy deficiency in sport in male athletes: A commentary on its presentation among selected groups of male athletes. International Journal of Sport Nutrition and Exercise Metabolism, 28(4), pp.364-374.
- Martinsen, M., Sherman, R.T., Thompson, R.A. and Sundgot-Borgen, J., 2015. Coaches’ knowledge and management of eating disorders: a randomized controlled trial. Med Sci Sports Exerc, 47(5), pp.1070-8.
- Caudill, B., 2018. Best Practices for Screening, Identification, and Referral of Female Collegiate Athletes with Disordered Eating.